➣ By Claudio Capelli
The safety and performance of medical devices prior to their use in clinical practice is currently demonstrated by the use of models. Computer models can contribute to creating a virtual environment for testing the efficacy of novel designs. Realistic simulations require information on the anatomy where the device will be employed, and on the physiologic conditions which will affect its mechanical behavior. Recent developments of modern 3-D imaging techniques, especially magnetic resonance (MR) and computed tomography (CT) imaging, make these aspects describable in socalled patient-specific models.
Patient-specific modeling has been used to develop new applications in the rapidly growing field of interventional cardiology, namely supporting the development of minimally invasive procedures for the treatment of valvular pathologies. In 2000, Professor Bonhoeffer demonstrated the feasibility of replacing a heart valve without resorting to an open-heart surgical operation: a biological valve, sewn into a stent, was crimped onto a catheter, inserted into a vein in the leg and guided to the heart. The device, Melody® Transcatheter Pulmonary Valve (Medtronic Inc.), offered children and adults suffering from a failing pulmonary valve a revolutionary option for treatment without being forced to undergo high-risk surgery. Additionally, in 2002, a transcatheter procedure was successfully performed in the aortic position (TAVI) as an alternative for dealing with the most common valve pathology in Europe and the U.S. Since then, this approach has seen groundbreaking success with more than 40,000 patients treated to date. However, the number of patients who could potentially avoid surgery is still limited by the number of devices which are rarely implantable in a patient population that varies in terms of morphology and dynamics.
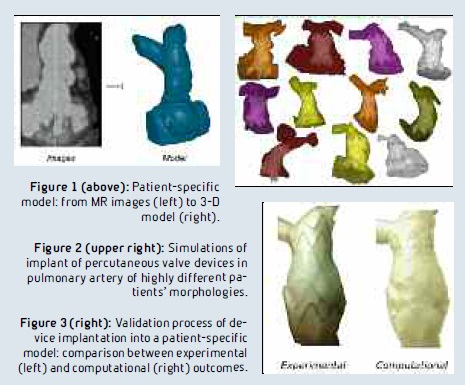
Hence, the pre-implantation assessment has become crucial. Next to well-established imaging techniques, we have developed patient-specific models in which we simulate the device implantation phase. MR and CT images are acquired and post-processed to create a 3-D model of the patient’s anatomy (Figure 1). One or more models of devices are then virtually implanted by finite element simulations. The final configurations are explored to assess the success of the procedure in a large population of patients (Figure 2). The best placement strategy and the distribution of stress were assessed. Results from the computational model are validated by bench experiments (Figure 3) and clinical results, supporting the reliability of the computational findings.
In general, the outcomes of these simulations can provide clinicians with further evidence on the feasibility of implants, as well as advise engineers about the risk of structural issues. At the University College London’s Institute of Cardiovascular Science and the Great Ormond Street Hospital for Children (London, UK), this technique has fostered a better understanding of episodes of device fractures, supported the first implant of a novel device for percutaneous pulmonary issues in a human, and explored the potential of minimally invasive alternatives for patients suffering from a failing bioprosthetic aortic valve.
In the future, our aspiration is a more extensive implementation of medical simulations in clinical practice. A multidisciplinary approach of this kind can open the doors to safer and more effective procedures tailored to the characteristics of every patient.
Claudio Capelli
Institute of Cardiovascular Science
University College London
United Kingdom
c.capelli@ucl.ac.uk
About Brenda Wiederhold
President of Virtual Reality Medical Institute (VRMI) in Brussels, Belgium.
Executive VP Virtual Reality Medical Center (VRMC), based in San Diego and Los Angeles, California.
CEO of Interactive Media Institute a 501c3 non-profit
Clinical Instructor in Department of Psychiatry at UCSD
Founder of CyberPsychology, CyberTherapy, & Social Networking Conference
Visiting Professor at Catholic University Milan.









