By Giuseppe Riva et al
Although frequent papers show that Virtual Reality (VR) has come of age for clinical and research applications, the majority of projects are still in the laboratory or investigation stage. In fact, according to the data that will be presented by Prof. Giuseppe Riva, Ph.D., Istituto Auxologico Italiano, Milan, Italy at the forthcoming CyberTherapy 2009 conference in Verbania, Italy – http://www.e-therapy.info – the real impact of VR in European behavioral health is still low:
- The penetration of VR in behavioral health care/research centers is minimal: around 0.5/1%
- The penetration of VR between behavioral health professionals is even lower: less than 0.001%
Why is VR more virtual than real for many health care practitioners? From the experience of the current researchers involved in this area it is possible to identify four major issues that are limiting the use of VR in psychotherapy and behavioral neuroscience:
- the lack of standardization in VR hardware and software, and the limited possibility of tailoring the virtual environments (VEs) to the specific requirements of the clinical or the experimental setting;
- the low availability of standardized protocols that can be shared by the community of researchers; the high costs (up to 100.000 ¤) required for designing and testing a clinical VR application;
- most VEs in use today are not user-friendly; expensive technical support or continual maintenance are often required.
To address these challenges, the Italian FIRB research project IVT2010 is developing NeuroVR (http://www.neurovr.org), a cost-free virtual reality platform based on open-source software, that allows nonexpert users to easily modify a virtual environment (VE) and to visualize it using either an immersive or non-immersive system. Now at its version 1.5, the original NeuroVR 1.0 received the 2007 Laval Virtual Science Award (http://www.lavalvirtual. org/) for the best Virtual Reality science application worldwide.
The majority of existing VEs for health care are proprietary and have closed source, meaning they cannot be tailored from the ground up to fit the specific needs of different clinical applications. NeuroVR addresses these issues by providing the clinical professional with a cost-free VE editor, which allows non-expert users to easily modify a virtual scene, to best suit the needs of the clinical setting.
Using the NeuroVR Editor (see Figure 1), the psychological stimuli/stressors appropriate for any given scenario can be chosen from a rich database of 2D and 3D objects, and easily placed into the pre-designed virtual scenario by using an icon-based interface (no programming skills are required). In addition to static objects, the NeuroVR Editor allows an overlay on the 3D scene of video composited with a transparent alpha channel. The editing of the scene is performed in real time, and effects of changes can be checked from different views (frontal, lateral and top).
Currently, the NeuroVR library includes different pre-designed virtual scenes, representing typical real-life situations, i.e., the supermarket, the apartment, the park. These VEs have been designed, developed and assessed in the past ten years by a multidisciplinary research team in several clinical trials, which have involved over 400 patients. On the basis of this experience, only the most effective VEs have been selected for inclusion in the NeuroVR library.
An interesting feature of the NeuroVR Editor is the possibility of adding new objects to the database. This feature allows the therapist to enhance the patient’s feeling of familiarity and intimacy with the virtual scene, i.e., by using photos of objects/ people that are part of the patient’s daily life, thereby improving the efficacy of the exposure. The second main component of NeuroVR is the Player, which allows the user to navigate and interact with the VEs created using the NeuroVR Editor.
The player offers a set of standard features that contribute to increasing the realism of the simulated scene. These include collision detection to control movements in the environment, realistic walk-style motion, advanced lighting techniques for enhanced image quality, and streaming of video textures using an alpha channel for transparency. The player can be configured for two basic visualization modalities: immersive and non-immersive. The immersive modality allows the scene to be visualized using a head-mounted display, either in stereoscopic or in mono-mode; compatibility with a head-tracking sensor is also provided. In the non-immersive modality, the virtual environment can be displayed using a desktop monitor or a wall projector. The user can interact with the virtual environment using either keyboard commands, a mouse or a joypad, depending on the hardware configuration chosen. A future goal of the developers is also to provide software compatibility with instruments that allow collection and analysis of behavioral data, such as eye-tracking devices and sensors for psychophysiological monitoring.
The current NeuroVR library includes a limited number of VEs addressing specific phobias (i.e. fear of public speaking, agoraphobia) and eating disorders. However, new pre-designed environments will be developed in the coming years: it is envisioned that the 250,000 people in the worldwide Blender user community will contribute to extend the NeuroVR library, developing new VEs which can be tailored by clinical professionals for a range of clinical and experimental needs.
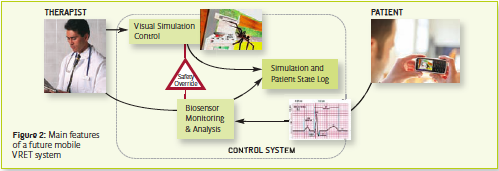
A final critical issue related to the use of VR in health care is the lack of availability of a VR system in the real life context of the patient: both the cost and the setting of the system limit its use to the health care center/hospital/therapist’s office. To overcome this issue, a VRML/X3D exporter for experiencing the environments on the Web and a player for PDAs and smartphones are planned features. The final goal is the development of a phone-based VR system able (see Figure 2):
- To present and structure emotionally relevant contents in a home setting;
- To verify the compliance of the patient and eventually alert the patient/therapist;
- To track in real-time the emotional level of the patient and record this for later assessment by the therapist;
- To provide feedback to the patient to enable him to cope with the environment’s contents;
- To automatically contact the therapist if the emotional level of the patient is higher than a preset cut-off value defined by the therapist.
Giuseppe Riva, Ph.D Andrea Gaggioli, Ph.D. Alessandra Gorini Ph.D. Istituto Auxlogico Italiano Italy giuseppe.riva@unicatt.it
About Brenda Wiederhold
President of Virtual Reality Medical Institute (VRMI) in Brussels, Belgium.
Executive VP Virtual Reality Medical Center (VRMC), based in San Diego and Los Angeles, California.
CEO of Interactive Media Institute a 501c3 non-profit
Clinical Instructor in Department of Psychiatry at UCSD
Founder of CyberPsychology, CyberTherapy, & Social Networking Conference
Visiting Professor at Catholic University Milan.