➣ By Lingjun Kong

Figure 1: Cell phones have become an integral tool in mobile health.
There is no doubt that the wireless revolution has had a remarkable impact on society and people worldwide. Inevitably, this technological trend has found itself becoming an essential progression and is rapidly spreading through the medical sector. Mobile Healthcare, commonly known as mHealth, is a term used to describe healthcare services provided by mobile communications and wireless technologies. Exploiting technologies such as mobile computing, medical sensors, and wireless communications, mHealth provides cost effective, easily accessible and overall better solutions for rehabilitation efforts. By allowing healthcare professionals, hospitals, and patients to interact on a more real-time basis, mHealth is dramatically changing and improving healthcare communications in rehabilitation therapy, training, and education.
Key Drivers
Value Proposition: Conscious of the value proposition and future of this emerging technology, large business corporations are jumping on board with mHealth healthcare services. High profile companies such as GE and Intel, UnitedHealth Group, Cisco, QUALCOMM, and many others are investing and launching products that help drive the next wave of wireless and mobile healthcare technology innovations. To provide better communication between patients and healthcare providers Microsoft’s HealthVault allows patients to store their healthcare information in one convenient location, Philips Healthcare’s wireless handheld devices offer patients in-home medical care services and GE’s QuietCare gives seniors a monitoring system that signals emergency situations to their healthcare providers. Various efforts are being undertaken to meet the demand of mHealth and many are joining together in collaboration. For example, the Wireless-Life Sciences Alliance is an organization that puts innovators and wireless health companies together with global leaders in healthcare and technology to accelerate business opportunities.
Patients: For many rehabilitation patients, the cost of physically traveling to a hospital for routine check-ups and services is escalated by their conditions and prevents them from getting needed treatments. Those with chronic conditions want to have access to quality healthcare services at the convenience of their own homes. By providing wireless tools for better patient care at home, healthcare professionals will enhance their management of ill patients with chronic conditions. According to The Department of Health and Human Services of the United States, 60% of individuals below the age of 65 have at least one chronic condition. As for the senior population over 65 years of age, about 77% have two or more chronic conditions. The amount of resources spent on chronic disease care accounts for an unnecessarily large proportion of healthcare expense in the US–about 90% of the gross domestic product. The growing number of patients and large amount of expenses spent towards their treatments makes the convenience of telecommunications vital.
Doctors: Doctors view the wireless capabilities of mHealth as a way to improve treatment for all patients. mHealth provides physicians with upgraded tools to treat patients. With wireless technology at their fingertips, they are better equipped to manage and diagnose patients to prevent disease. Doctors favor these improvements in mHealth that allow them to provide treatments and services and efficiently meet overwhelming demands from patients.
Innovators: Because the mHealth is a relatively new field, it provides many frontiers for researchers to explore and attracts many researchers who want to improve it. To these innovators, mobile technology offers challenges for them, pushing them to take the existing technologies to the mobile level.
Applications
Innovations in wireless and mobile healthcare have grown surprisingly fast. By allowing realtime interaction between clinicians and patients, mHealth is enabling a shift in healthcare communications. Many forms of mobile application have existed in the medical sector such as patient scheduled doctor visits, access to copies of patient medical records, remotely monitored patient data and locations of appropriate hospitals based on requirements, rating etc. Presently, a wave of wireless applications is surging including vital sign monitoring devices that can track weight, blood pressure, heart rate, and pulse oximetry and home health gateways that help bridge patients’ homes and healthcare providers. From the intricate high-end technologies to the simple free application on the iPhone, mHealth is spreading to both professional and casual users. Moreover, mobile devices are capable of playing a key role in remote management of patients with rehabilitation conditions. Patients can collect data from biometric devices at remote locations and upload and send the physiological data to their physicians where it could be electronically monitored. Physicians can then evaluate the data and take action when necessary.
iMAT, Mental Armor Training, is a mobile neuropsychological training program that serves to enhance soldiers’ abilities to form accurate interpretations of the events they experience during deployment and in everyday life. The application permits users to complete a series of exercises designed to improve judgment during stressful situations. The program provides different levels, each asking the user to apply their training to personal experiences. iMAT takes advantage of mobile platforms during overseas deployment to aid in the study of U.S. Army National Guard to determine appropriate physiological and cognitive interventions.
CardioNet, a mobile cardiac telemetry technology provides ambulatory, continuous, realtime outpatient management solutions for patients with cardiopathy. It utilizes wireless medical technology to provide a portable wireless monitoring device to keep track of patients’ heartbeats 24 hours a day for an extended period of time. CardioNet’s initial efforts are focused on the diagnosis and monitoring of cardiac arrhythmias or heart rhythm disorders, with a solution that markets it as Mobile Cardiac Outpatient Telemetry MCOT™. The newer enhanced version allows physicians to access more in-depth data to better diagnose atrial fibrillation, abnormal beats, and ventricular tachycardia (a potentially dangerous fast heartbeat). With the trended heart rate data provided by MCOT™, physicians are able to make clear and efficient clinical decisions to their patients based off this normally unattainable data at the hospital.
The Power of the Cell Phone
The mobile phone has become the most favored platform for innovation in the medical sector. With 4-billion total mobile subscribers, cell phones are not only growing in popularity, but also in computing capabilities. New features are added everyday making the cell phone a diverse personalized miniature computer. The inventions of medical professionals and researchers are turning the cell phone into a mobile hospital.
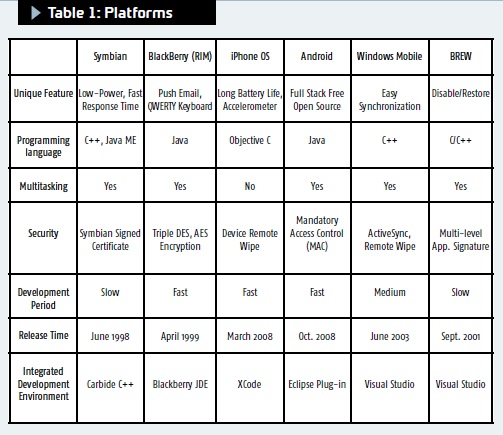
Platforms (Devices): From the mature platforms such as Symbian, BREW and Windows Mobile, to the current dominators of the mobile applications such as Android and iPhone, cell phone platforms have presented a diverse environment available to medical researchers (see Table 1).
Android: Growing at a rapid pace, Android is a hot phone platform built on top of the Linux kernel, and has come a long way in a relatively short time. Although at an early stage of its life, Android will certainly have a dominating presence in the near future. Launched in November 2007, Android, owned by Google, and now under the control of the Open Handset Alliance (OHA), promotes a free open-source operating system based on Linux for mobile devices. As the only full-stack free open source operating system, opening access to all levels of the operating system, Android offers third party developers opportunities to write applications in Java programming by utilizing Android API. Compared to other platforms, it not only is able to access the multitude of Google applications, but also does not require re-development for porting among different cellular devices. A significant feature that differentiates Android from the iPhone platform is that Android officially supports background processes in third-party applications.
iPhone: With its numerous applications, the iPhone has become a household name even in the medical world. Currently, no other phone can compare to its powerful distribution channel and social impacts to influence millions of everyday consumers and clinicians. From casual widgets, such as a drug interactive checker, clinical reference tools, medical news, and contact information for physicians, pharmacies and hospitals, to more sophisticated services such as a stethoscope, a game to diagnose diseases and an emergency radio, patients and doctors are enjoying these interactive tools at their convenience. The iPhone has not only evolved into more than a consumer electronics device due to its attractive interface, applications marketplace, and consumer appeal, it has also been heavily integrated into the medical field via high resolution medical images and various software applications.
Challenges
Mobile technology in the healthcare field is still in an early stage and requires a selection of hardware upgrades, such as ultra- low power usage, computation, and communication for overall extended battery life. However, the main issues revolve around security, interoperability, and regulatory compliance areas.
Security: The privacy of patients’ data becomes a pressing issue in the development of mHealth technology. Since most casual services only offer a username-password combination to access sensitive data, many users are cautious about giving away the needed information that is required of them. The relative ease of leaking personal information, including identification and medical histories, makes the need of well-regulated security policies extremely important as mHealth continues to proliferate.
Interoperability: Due to its fast growth and relatively new technologies, mHealth services do not boast interoperability, meaning services provided by one platform may not be understood or transferred to services offered by another. Medical devices are frequently not configured in the same way by the device vendors and as they are by the network infrastructure. Although cellular, Blue-Tooth, and Wi-fi standards have been well-established, developing technologies are constantly shifting and standards will take time to become concrete.
Regulatory compliance: To regulate the flood of new medical services in mHealth, the Federal Communications Commission (FCC) and the Food and Drug Administration (FDA) claim jurisdiction over mobile devices in healthcare. The FCC must approve all upcoming mobile devices before they can be released; while the FDA must approve all medical devices before entering the market. Other healthcare regulations, such as HIPPA, also need to be taken into consideration during any deployment of mHealth devices.
Regardless of the challenges facing it, the numerous opportunities and medical benefits that the mobile platforms offer will be refined and will provide many advantageous solutions to doctors and patients. The new platforms are significantly shifting and improving the quality, convenience and accessibility of healthcare.
Lingjun Kong, M.S.
Virtual Reality Medical Center
U.S.A.
lkong@vrphobia.com
www.vrphobia.com
➣
About Brenda Wiederhold
President of Virtual Reality Medical Institute (VRMI) in Brussels, Belgium.
Executive VP Virtual Reality Medical Center (VRMC), based in San Diego and Los Angeles, California.
CEO of Interactive Media Institute a 501c3 non-profit
Clinical Instructor in Department of Psychiatry at UCSD
Founder of CyberPsychology, CyberTherapy, & Social Networking Conference
Visiting Professor at Catholic University Milan.






