By Hayoung Park, YuCheong Chon & Kun-Ho Yoon
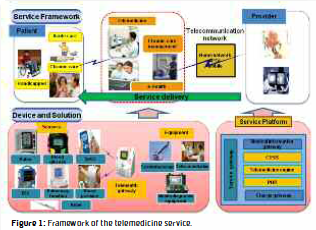
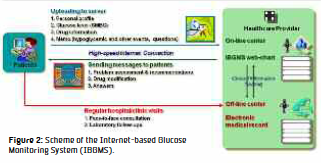
Telemedicine is the conversion technology which is expected to improve quality of care while improving the efficiency of the delivery of care, and the management of chronic conditions with the technology is of particular interest as the size of the aged population increases rapidly (Figures 1 and 2). However, attempts to introduce telemedicine in South Korea during the past 20 years have been largely unsuccessful due to various reasons: regulations designed for traditional medicine, immature technology, physician reluctance to change, and lack of patient willingness to pay for and adapt to the new mode of care. As regulatory issues and technological limitations are overcome through the Korean government’s efforts and technology advancement, establishing a sustainable revenue model and designing a service that attracts patients have become important factors for the successful implementation of telemedicine. Patients’ willingness to pay has a particular significance in South Korea since national health insurance coverage allows patients easy access to specialty care in clinics and hospitals, although patients’ waiting time is long and consultations with doctors are insufficient in large teaching hospitals preferred by patients. In a conjoint survey conducted through face-to-face interviews, we asked patients residing in the Seoul metropolitan area who visited medical school affiliated tertiary care hospitals and clinics for diabetes care about their preferences among telemedicine service alternatives where the alternatives differed in price and nine attributes derived from dimensions of service quality: type of service provider, service scope, personalization of consultation, service hour, reply time, assurance of service, type of telecommunication platform, system reliability, and level of confidentiality assurance. We analyzed a total of 118 responses with the rank-ordered logit model based on the random utility model to find the patients’ value and preferences for each attribute of telemedicine service for diabetes management.
We found that all 10 attributes of diabetes management care using telemedicine significantly affected patients’ valuations and preferences. Price was the most important attribute for patients in choosing a telemedicine service alternative. The next most important attributes were: the comprehensiveness of service scope that includes care for other complicating and comorbid conditions and consultations for diet and exercise as well as glucose control, the availability of mobile phone-based service delivery, general hospital-based providers, and assurance of services. We found that patients were less concerned about the reply time and information security than the other attributes. Although patients were most concerned about price, they were willing to pay a monthly fee of over $10 USD to attain the service attributes they value such as the comprehensiveness of service scope, mobile-phone based service, and general hospital-based provider. We also found that demographic and disease characteristics made a difference in patients’ valuations and preferences for the attributes. Females were more sensitive to assurance than males; older respondents were more accepting of office-hour only service than younger respondents; and respondents with higher education preferred Internet-based service more than others. Patients with complications or comorbidities cared more about general hospital-based providers for the assurance of care quality and mobile-phone based services for easier access to care than other respondents did.
We draw four implications from the study findings for the formulation of an adoption policy and the design of services using telemedicine. First, potential beneficiaries of the technology were most concerned about price among the service attributes studied, and the government or insurer may need to consider covering services with evidence of costeffectiveness of the service. Second, the very feature of the technology – indirect delivery of care through telecommunication devices – strengthened the importance of the quality domain of service assurance, and service developers may need to institute a mechanism in their service design that ensures patients’ trust. Third, it appeared that the levels of confidentiality and system reliability threshold of 1-5% failure were acceptable to patients although information safety and confidentiality have been indicated as obstacles in the adoption of information and communications technology (ICT) in healthcare, and researchers may need to quantitatively study patient preferences and concerns to attain knowledge that can guide the design of services. Lastly, patients’ demographic and disease characteristics influenced their preferences, and policy makers and service developers may need to approach different patient groups with different strategies tailored to their needs and preferences.
Author Notes: The article is based on the study published in Telemedicine and e- Health: Park H, Chon Y, Lee J, Choi I, Yoon K. Service design attributes affecting diabetic patient preferences of telemedicine in South Korea. Telemedicine and e-Health 2011;17:442-451.
About Brenda Wiederhold
President of Virtual Reality Medical Institute (VRMI) in Brussels, Belgium.
Executive VP Virtual Reality Medical Center (VRMC), based in San Diego and Los Angeles, California.
CEO of Interactive Media Institute a 501c3 non-profit
Clinical Instructor in Department of Psychiatry at UCSD
Founder of CyberPsychology, CyberTherapy, & Social Networking Conference
Visiting Professor at Catholic University Milan.